Bringing a new drug treatment from the lab to your local pharmacy is a long and complex journey. At first glance, it may seem like a miraculous process where researchers discover a breakthrough compound, and suddenly, it appears on pharmacy shelves. In reality, a rigorous system ensures that each new medication is both safe and effective. This article explores how a promising chemical in a laboratory transforms into a prescription medication that healthcare professionals trust and patients rely on, covering every step from initial discovery to final distribution.
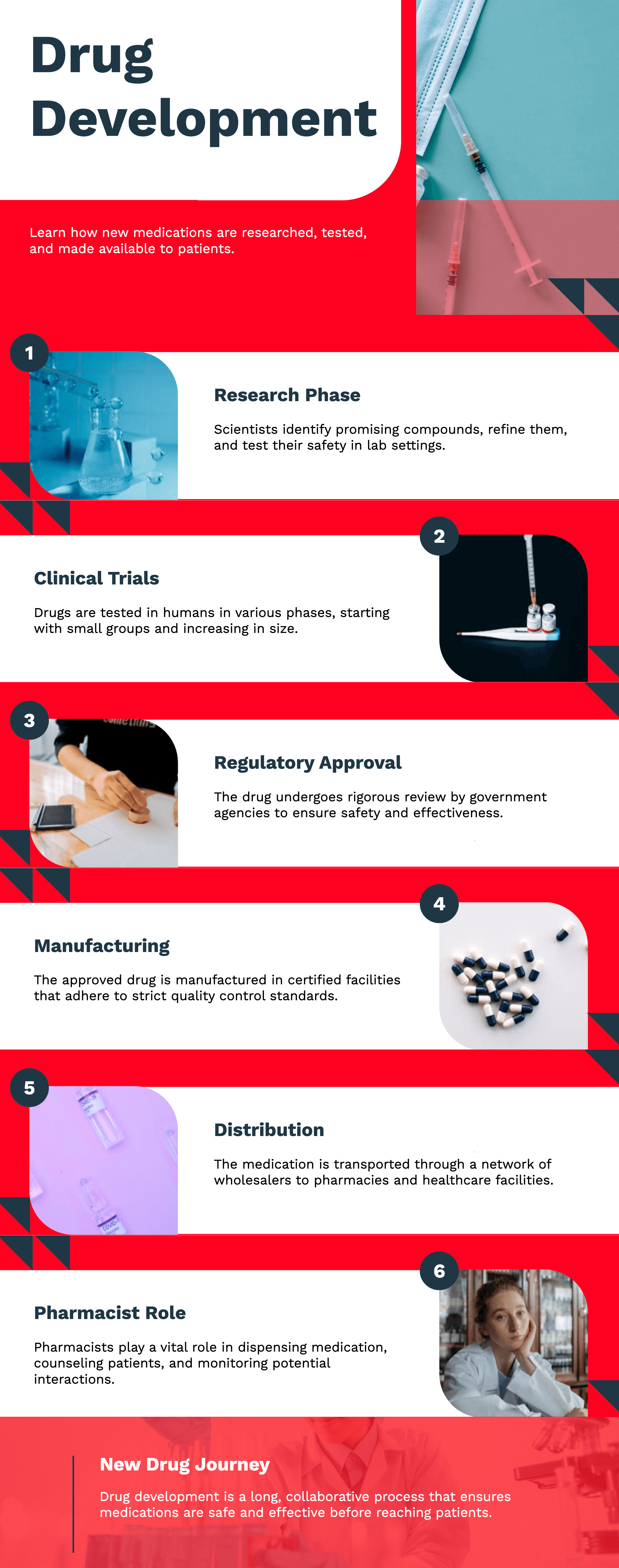
Researchers worldwide continuously search for new drug treatments. The process typically begins when scientists observe something noteworthy in nature, existing drugs, or advanced computer simulations. They may study how a specific molecule interacts with cells or proteins in the body. When they identify a promising potential to improve health, the molecule becomes a "lead compound." This potential drug then undergoes multiple tests to determine if it warrants further exploration.
Refining the Lead Compound
Once a lead compound is identified, scientists refine it by modifying its chemical structure, testing different doses, and observing its effects on lab-grown cells or animal subjects. The primary objective is to detect any harmful effects or adverse chemical behaviors that could pose risks to humans. If the compound continues to show promise while avoiding major safety concerns, it advances to clinical trials.
Early Safety Assessments
In this preliminary phase, toxicology tests play a critical role. These tests help determine whether the new compound causes significant organ damage, cell toxicity, or other side effects. Identifying potential risks early allows scientists to make necessary modifications, ensuring the safety of future clinical trial participants. This approach not only conserves time and resources but also safeguards human volunteers as the drug progresses to the next stages.

Clinical trials are the backbone of new drug development. They involve multiple phases, each designed with specific objectives, participant groups, and stringent guidelines. These studies are carefully structured and monitored to ensure that the collected data accurately reflects the drug’s effects in humans.
Phase 1 Trials
Phase 1 trials mark the first occasion where a new drug is tested on a small group of participants, usually healthy volunteers. However, for severe illnesses like cancer, the trials may include patients instead. The primary objectives of Phase 1 trials are:
Because this is the initial testing stage in humans, researchers closely monitor participants for any unexpected effects. If serious issues arise, the trial may be halted or adjusted.
Phase 2 Trials
Phase 2 trials involve a larger group of participants who have the condition the drug is intended to treat. The key objectives at this stage include:
Phase 3 Trials
Phase 3 trials expand the study to hundreds or even thousands of participants across multiple clinical sites worldwide. This scale is essential for evaluating the drug’s broader impact and identifying rare side effects. The main objectives include:
If the Phase 3 results confirm the drug’s efficacy and safety, the sponsoring company compiles the data for regulatory review.

Before a new drug enters the market, it must undergo a rigorous review by regulatory authorities. These organizations ensure that only medications meeting high safety, quality, and effectiveness standards reach consumers.
Role of Regulatory Authorities
Regulatory bodies such as the FDA (United States), EMA (Europe), NMPA (China), and TGA (Australia) evaluate new drug applications. The submitted data includes:
Expert teams—including medical doctors, statisticians, chemists, and pharmacologists—scrutinize the application. They may request additional studies or clarifications, with the approval process taking months or even years, depending on data complexity and revisions.
Post-Market Surveillance
Even after approval, regulatory authorities continue monitoring the drug’s safety. Healthcare professionals and patients report adverse reactions, which can lead to further investigations, warnings, or even drug recalls if necessary.

Once regulatory approval is granted, manufacturing shifts into full-scale production, ensuring consistent quality across all batches.
Facility Standards
Pharmaceutical companies must produce new drug treatments in certified facilities following Good Manufacturing Practices (GMP). These regulations cover:
Regulatory authorities conduct routine inspections, and non-compliance can lead to penalties, recalls, or production shutdowns.
Packaging and Labeling
Each manufactured dose undergoes packaging and labeling, which includes:
Proper labeling prevents medication errors and ensures patient safety.
Once final quality checks are complete, the medication is distributed to hospitals, clinics, and pharmacies through a regulated supply chain.
Wholesale Networks
Most pharmaceutical products go through wholesale distributors before reaching healthcare facilities. These wholesalers handle large inventories and ensure timely deliveries, including cold-chain logistics for temperature-sensitive drugs. More broadly, medications are transported under controlled conditions to maintain efficacy.
Pharmacist Guidance: Your Last Line of Defense
At the pharmacy, pharmacists verify prescriptions, check for potential drug interactions, and provide guidance on proper medication use. Patients are encouraged to ask questions, such as:
Following pharmacist guidance helps ensure the safe and effective use of new medications.
New drug treatments are only as effective as the healthcare teams that prescribe and monitor them. Physicians, nurses, and pharmacists work together to optimize patient outcomes.
Collaborative Care in Medical Facilities
In hospitals and clinics, healthcare teams coordinate to:
This continuous collaboration ensures that treatments remain safe and effective for patients.

From its earliest discovery in a laboratory to its availability at pharmacies, every new drug treatment undergoes an extensive process to ensure safety, efficacy, and quality. Researchers conduct rigorous clinical trials, regulatory authorities review extensive data, and manufacturers maintain high production standards. Even after a drug is approved, ongoing monitoring ensures patient safety. This intricate system may be lengthy, but it exists to provide reliable and effective medical solutions worldwide.
It often takes 10 to 15 years from initial research to final approval. This includes discovery, preclinical testing, multiple clinical trial phases, and regulatory reviews.
Failure can occur at any phase. If the data shows the drug is unsafe or not effective, the trial may stop, or researchers may modify the compound before continuing. Some drugs never make it past the testing stage.
Generic drugs are typically copies of brand-name drugs whose patents have expired. They must prove bioequivalence to the original, but they do not require the same large-scale clinical trials since safety and efficacy data already exist.
Companies invest heavily in research, clinical trials, and regulatory steps. They set initial pricing to recover these costs. Over time, prices may drop, especially once generic versions become available.
Yes. Many patients join trials to access experimental treatments, especially if existing therapies are not working. Each trial has specific eligibility requirements based on the drug’s target condition and the patient’s health status.
 26.02.2025
26.02.2025