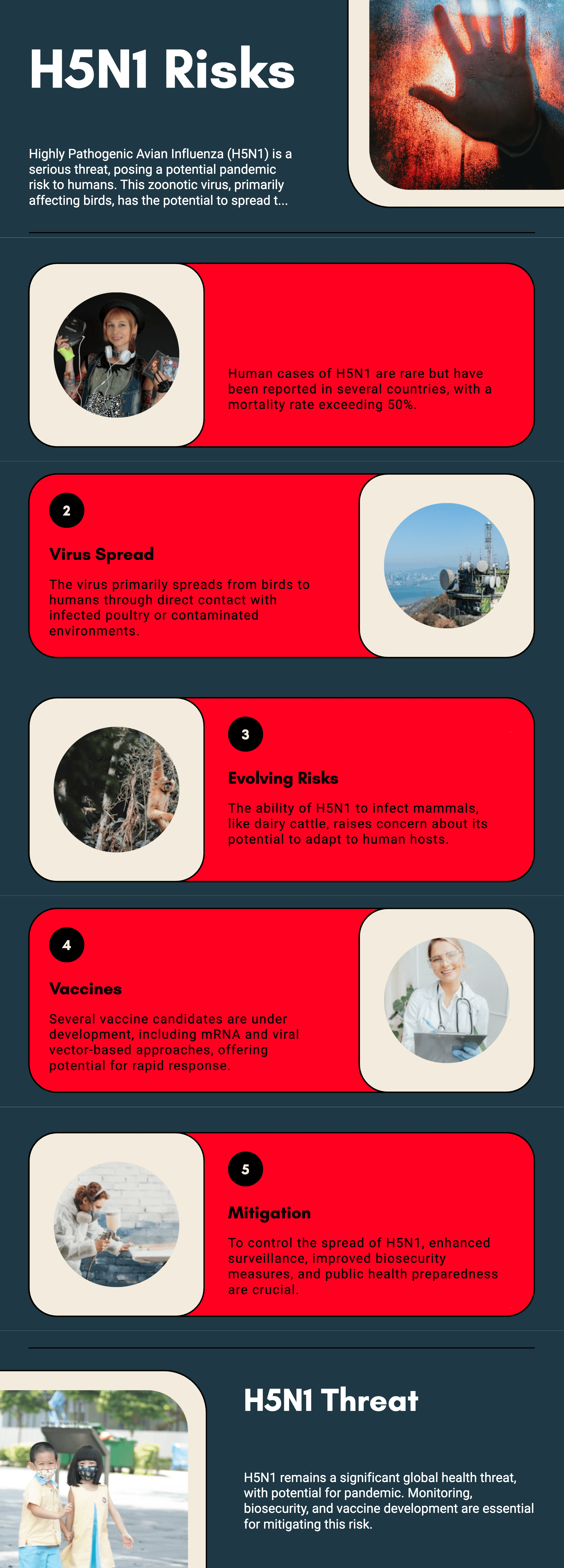
Highly Pathogenic Avian Influenza (HPAI) A(H5N1) is a severe and often fatal zoonotic virus with pandemic potential. First identified in humans in 1997, its sporadic but deadly outbreaks have raised concerns among global health agencies. As the virus continues to evolve, monitoring its transmission, understanding risk factors, and advancing vaccine development are critical to preventing a public health crisis.
This article explores the evolving risks of H5N1 in humans, recent outbreaks, transmission pathways, and the progress in vaccine research.
H5N1 is an influenza A virus primarily affecting birds but capable of jumping to humans and other mammals. The virus spreads through direct contact with infected poultry, contaminated environments, or, in rare cases, human-to-human transmission.
Key Characteristics of H5N1
H5N1 remains a persistent global health threat, with recent outbreaks reported in multiple regions.
Notable Outbreaks in 2023-2024
Emerging Trends in Human Cases
H5N1 primarily spreads from birds to humans through:
Direct Contact: Handling infected poultry or consuming undercooked bird products.
Airborne Exposure: Inhaling virus-laden particles from bird droppings or contaminated surfaces.
Mammalian Spillover: Recent cases in dairy cattle suggest new transmission routes, necessitating increased biosecurity.
Human-to-Human Transmission: A Growing Concern?
While limited, there have been isolated cases of human-to-human transmission. A 2023 study found that viral mutations in certain strains have enhanced infectivity in human respiratory cells. However, sustained transmission remains unlikely in its current form.
Several factors contribute to H5N1's potential to trigger a global outbreak:
The virus’s ability to infect mammals suggests a growing risk of adaptation to human hosts. Reports of H5N1 in dairy cattle and wild mammals indicate potential for further evolution.
Unlike seasonal influenza, humans have little to no pre-existing immunity to H5N1. This makes infections more severe and raises concerns about their pandemic potential.
If H5N1 co-infects an individual already carrying a human flu strain, the viruses could swap genetic material, creating a novel, highly transmissible strain.
Many regions lack robust monitoring systems, allowing the virus to spread undetected among poultry, wildlife, and even livestock.
Efforts to develop vaccines against H5N1 have accelerated, with several candidates showing promise.
Current H5N1 Vaccines
| VACCINE CANDIDATE | TYPE | STATUS | KEY FEATURES |
|---|---|---|---|
| QIVc (Cell-based) | Inactivated | Approved for stockpiling | Broad-spectrum protection (primarily for H3N2, H1N1) |
| mRNA-1011 | mRNA | Phase 1 trials | Adaptable to new variants (not specific to H5N1) |
| J&J Ad26-based | Viral vector | Preclinical | Long-lasting immunity |
| Sanofi H5N1 | Recombinant | Licensed (Not in development) | Used for emergency preparedness |
Challenges in Vaccine Development
To reduce the risk of an H5N1 pandemic, coordinated efforts are needed:
Enhanced Surveillance
Poultry and Livestock Biosecurity
Public Health Preparedness
Accelerated Vaccine Development

H5N1 remains a formidable global health threat, with its ability to infect mammals raising pandemic concerns. While human cases remain rare, the virus's potential for adaptation necessitates proactive surveillance, rapid response strategies, and continued investment in vaccines.
The recent detection of H5N1 in dairy cattle and human workers highlights the evolving nature of the virus. Although no sustained human-to-human transmission has been observed, the risk remains. Strengthening biosecurity, improving surveillance, and advancing next-generation vaccines are crucial in preventing a future pandemic.
H5N1 rarely spreads between humans. While isolated cases have occurred, sustained human-to-human transmission has not been confirmed.
Symptoms range from mild fever and cough to severe pneumonia, respiratory failure, and death. Some infections remain asymptomatic.
Antiviral drugs like oseltamivir (Tamiflu) can help if administered early. However, drug resistance has been reported in some strains.
Avoid contact with sick or dead birds, cook poultry thoroughly, and follow hygiene practices when handling animals.
Several vaccines have been developed and stockpiled for emergency use, but none are widely available for public distribution yet.
 14.02.2025
14.02.2025