Gene editing is shaping the future of medicine and agriculture. It involves changing a species’ DNA to remove unwanted traits or introduce new ones. Thanks to CRISPR gene editing, we have gained a powerful tool that is faster, cheaper, and more precise than previous techniques. Yet, with all these promises come serious questions about safety, fairness, and the moral limits of altering life’s blueprint. In this article, we will explore the fundamentals of gene editing, its potential benefits, the ethical concerns it sparks, and how regulations try to keep pace with rapid scientific developments.
At its core, gene editing aims to modify an organism’s DNA in a targeted way. This can mean adding a new gene, removing a problematic gene, or “turning off” certain genetic instructions. For many years, scientists used tools like zinc-finger nucleases and TALENs to cut DNA at exact spots. But the high cost and complexity of these methods limited their widespread adoption.
Defining Gene Editing
Gene editing is a set of methods we use to make intentional changes in DNA. These changes can prevent diseases or improve a crop’s resistance to pests. When scientists alter the DNA in eggs, sperm, or embryos, those modifications could be passed down to future generations. This possibility of heritable changes lies at the heart of the ethical debate because it has the power to shape not just individual lives, but entire species over time.
Brief Overview of Key Techniques
Before CRISPR gene editing arrived, older tools worked but often lacked precision. They also took longer to produce the right kind of cuts in a strand of DNA. With the introduction of the CRISPR-Cas9 system, everything changed. Suddenly, labs worldwide could target genes with relative ease. This surge in efficiency allowed more research, faster breakthroughs, and greater interest in using gene editing to solve global challenges.
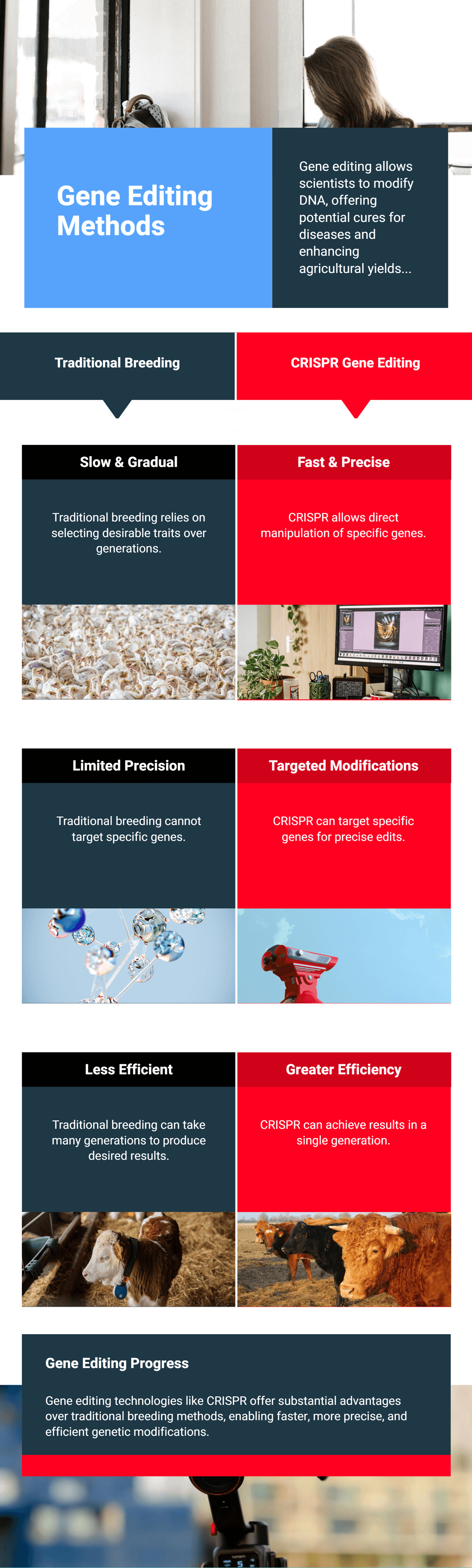
The concept of altering genetic traits is not new. Humans have been selectively breeding plants and animals for thousands of years to create stronger, healthier, or more desirable traits. Early farmers chose seeds from the most robust crops. Livestock breeders mated animals that had the best features. Over the centuries, this slow selection process led to dramatic improvements. But it was largely guesswork.
From Early Selective Breeding to Modern CRISPR
Traditional breeding paved the way for modern genetics. As we learned the structure of DNA in the mid-20th century, scientists discovered how genes control traits. This knowledge set the stage for the first experiments in genetic engineering, which used recombinant DNA techniques to insert genes from one organism into another. Today, with CRISPR, we can make precise edits to existing DNA sequences in ways that were unimaginable a few decades ago. This dramatic shift has opened doors to curing genetic diseases and boosting agricultural yields. Yet it also leaves us wondering: Just because we can alter DNA, should we?
CRISPR stands for Clustered Regularly Interspaced Short Palindromic Repeats, a fancy phrase for repeating patterns of DNA that are part of a bacteria’s immune system. Researchers discovered that bacteria use the CRISPR system to “remember” viral invaders and cut them out if they try to infect again. From this natural mechanism, scientists developed a method to guide the Cas9 enzyme to any chosen DNA segment. The Cas9 enzyme then makes a precise cut. Once the cut is made, we can remove, correct, or replace that piece of DNA.
The beauty of CRISPR is its simplicity and flexibility. By designing a short piece of RNA that matches the target gene, researchers can direct Cas9 with remarkable accuracy. This streamlined process has revolutionized gene editing, making it more accessible to labs of all sizes. It is now easier than ever to perform experiments on animals, plants, and even human cells, opening doors to countless possibilities. However, such power requires careful handling to avoid mistakes and unintended consequences.
The range of benefits from CRISPR gene editing goes beyond what many of us dreamed possible. In the medical field, we see potential cures for inherited disorders like cystic fibrosis, muscular dystrophy, and certain forms of cancer. Instead of using gene therapy on living tissues, which might be harder to control, future treatments might tackle the disease at its genetic root.
Revolutionizing Healthcare
By pinpointing and deactivating harmful mutations, CRISPR could reduce or even eliminate genetic conditions. There are ongoing clinical trials examining how safe and effective these therapies could be. While the results are still emerging, early signs suggest we may be on the brink of a new medical era. This includes possible treatments for sickle cell disease, where corrected cells can produce healthy hemoglobin instead of the abnormal version.
Personalized Treatments
Medical researchers also see the possibility of personalizing therapies. Using CRISPR, doctors could tailor medicine to a patient’s unique genetic profile. Think of a future where cancer treatments are customized to your tumor’s DNA, or where damaged heart cells get repaired on a genetic level. If done responsibly, these breakthroughs promise a leap forward in disease prevention and patient care.
 Risks and Limitations
Risks and LimitationsWhile CRISPR has undeniable potential, it is not perfect. There can be off-target effects, meaning the Cas9 enzyme might cut the wrong spot on the DNA. Even small unintended changes can lead to serious health problems over time. Researchers are working on improving the accuracy, but these risks underscore the need for thorough testing and oversight.
Unexpected Mutations
An added concern is the possibility of mosaicism, where some cells carry the edited gene while others do not. This imbalance can cause unpredictable outcomes. For instance, if gene editing is done at the embryonic stage, only certain cells in the developing organism might pick up the change. This can make it harder to predict and control the eventual results of an edit.
Ethical Dilemmas
There are also worries about using gene editing for non-medical enhancements. If CRISPR technology becomes widespread, a new social divide could emerge between those who can afford genetic “upgrades” and those who cannot. This raises complex questions about fairness, equality, and what kind of society we want to build with powerful biotech tools at our fingertips.
The idea of editing genes in human embryos is where the controversy heats up. Changing an embryo’s DNA could prevent diseases from ever appearing. Yet it also means that any changes we introduce would get passed down to future generations. Critics argue that scientists and governments need more robust guidelines before diving into such experiments. Others worry about a “slippery slope” leading to designer babies, where parents pick traits like eye color or intelligence.
On the other hand, supporters say that if we can reduce suffering by removing disease-causing mutations, it might be unethical not to use the technology. This is the heart of the ethical debate behind DNA modification: balancing the desire to eliminate human suffering with the need to protect human dignity and diversity. Most experts agree that broad public discussions, along with clear regulations, are essential to chart a responsible path forward.
Gene editing in agriculture aims to improve food security. We can develop crops that resist pests, need fewer chemicals, and yield more food. For instance, scientists are looking into boosting a plant’s tolerance to temperature changes and drought. This is critical in a world facing climate change. If we can improve crop resilience, we can help communities avoid food shortages.
Yet public opinion on genetically modified organisms (GMOs) remains divided. While some see genetically edited crops as a promising solution to famine and malnutrition, others argue we might disturb natural ecosystems. Concerns over the safety of gene-edited foods add another layer to the debate, making transparency and long-term studies important for building public trust.
Governments worldwide are grappling with how best to regulate CRISPR and gene editing. Some nations, such as the United States, classify gene-edited foods differently than those produced using older genetic engineering techniques. Meanwhile, the European Union has stricter rules, seeing little difference between conventional GMO methods and newer gene editing approaches.
Agencies like the U.S. Food and Drug Administration (FDA), the European Food Safety Authority (EFSA), and others work to ensure public safety. But technology often moves faster than regulations can keep up. As CRISPR improves, lawmakers face pressure to adapt quickly. The challenge is to find a balance that encourages innovation while preventing misuse. International cooperation is also crucial because DNA-altered organisms can cross borders, and decisions in one country can affect global markets.
Many people first heard about CRISPR when scientists in China announced they had edited the genes of human embryos. Public reaction ranged from excitement to alarm. The media’s portrayal of gene editing often oversimplifies the technology, or swings between doomsday scenarios and miracle cures.
Building public trust requires honesty about benefits, risks, and uncertainties. Health organizations, biotech companies, and governments need to share data openly. Clear communication can help people understand how CRISPR works and why it may matter to them. The public also needs a say in deciding the limits of gene editing. Since these decisions could alter the fabric of humanity, democratic debate is vital.
Scientists are exploring new twists on CRISPR, such as base editing and prime editing, which could further reduce off-target effects. These methods allow even more precise changes, converting one DNA “letter” to another without introducing a full cut. As these techniques mature, the cost of gene editing may drop further, and more people could gain access to life-changing treatments.
Another area to watch is the combination of CRISPR gene editing with stem cell research. By editing stem cells to remove mutations, doctors may one day grow healthy tissues and organs tailored to patients. This could revolutionize transplants and speed up the development of effective therapies.
Our ability to edit genes is advancing at an astonishing pace. It offers hope for treating diseases that were once considered incurable and could bolster our food supplies in a warming world. Yet these promises come bundled with questions about unintended consequences, fairness, and moral limits. As with any transformative technology, it is vital that we balance innovation with responsibility. Governments, scientists, and the public must work together to shape how CRISPR gene editing unfolds. If we do this right, gene editing may help us overcome some of humanity’s biggest challenges while ensuring we protect the diverse tapestry of life.
Different countries have different regulations. While research is permitted in many places, clinical use on humans may be more restricted. Laws and guidelines keep evolving as science advances.
Several clinical trials are underway, but it could take years before treatments are widely available. Researchers need time to confirm safety, effectiveness, and long-term outcomes.
In theory, yes, but regulations in most countries prohibit using CRISPR for non-medical enhancements in humans. The debate continues over what is ethically acceptable.
So far, no credible evidence suggests gene-edited foods are harmful. Still, long-term studies and transparent safety assessments are essential to reassure the public.
Off-target edits can occur, and they might lead to unexpected health or environmental issues. Researchers use various screening methods to reduce these risks, but ongoing caution is necessary.
 11.02.2025
11.02.2025