Immunotherapy is transforming the way cancer is treated, offering hope to patients by harnessing the body’s natural defense system. In this comprehensive guide, we explore the mechanisms, types, benefits, and challenges of immunotherapy in cancer treatment.

Immunotherapy is a type of cancer treatment that leverages the immune system to fight cancer. Unlike traditional therapies like chemotherapy or radiation, immunotherapy enhances the body’s natural defenses, allowing it to identify and destroy cancer cells more effectively.
The immune system plays a critical role in maintaining the body’s health. It detects and eliminates abnormal cells, including cancerous ones. However, cancer cells can evade detection by:
Immunotherapy addresses these challenges by boosting the immune system's ability to target and destroy cancer cells.
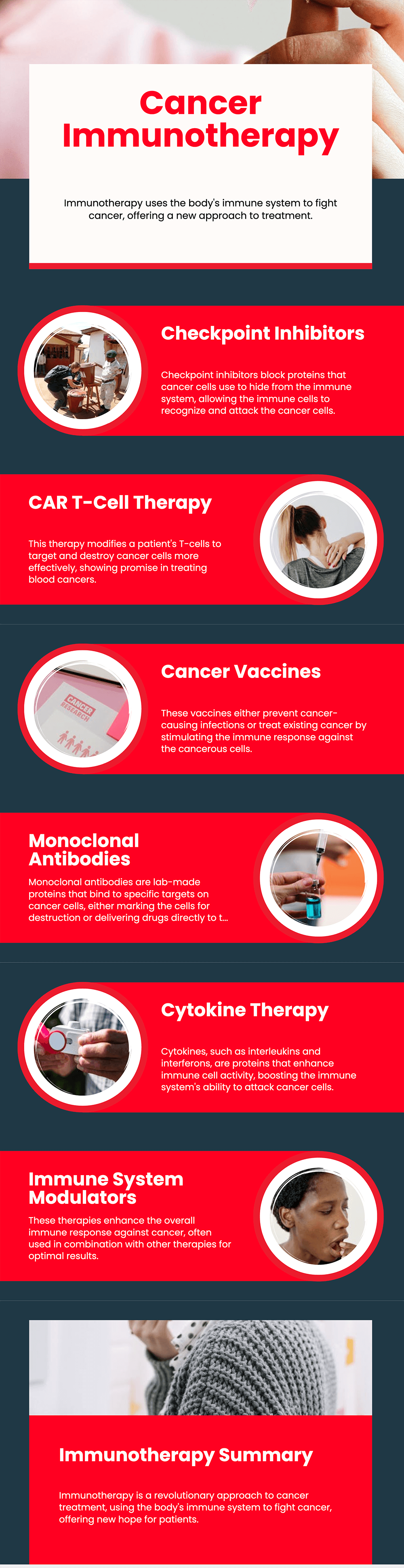
Checkpoint inhibitors block proteins used by cancer cells to hide from immune cells. These drugs help immune cells recognize and attack cancer. Examples include:
Chimeric Antigen Receptor (CAR) T-cell therapy modifies a patient’s T-cells to better recognize and attack cancer. This personalized approach has shown promise in treating blood cancers like leukemia and lymphoma.
Cancer vaccines either prevent cancer-causing infections (e.g., HPV vaccine) or treat existing cancer by stimulating an immune response.
Monoclonal antibodies are lab-made proteins that bind to specific targets on cancer cells. Some antibodies mark cancer cells for destruction, while others deliver drugs or radiation directly to the tumor.
Cytokines, such as interleukins and interferons, are proteins that enhance immune cell activity. Cytokine therapy boosts the immune system’s ability to attack cancer cells.
These therapies enhance the overall immune response against cancer. Examples include interleukin-2 (IL-2) and interferon-alpha.
Immunotherapy can be delivered through various methods, depending on the type of treatment and cancer being targeted:
While immunotherapy offers significant benefits, it can also cause side effects, including:
Most side effects are manageable with prompt medical attention.
Immunotherapy is not suitable for all cancer patients. It is most effective for:
Research is advancing rapidly, with promising developments such as:
| TYPE | MECHANISM | EXAMPLES | CANCER TYPES |
|---|---|---|---|
| Checkpoint Inhibitors | Block proteins that inhibit immune cells | Pembrolizumab, Ipilimumab | Melanoma, Lung Cancer |
| CAR T-Cell Therapy | Modify T-cells to attack cancer | Kymriah, Yescarta | Leukemia, Lymphoma |
| Monoclonal Antibodies | Bind to cancer-specific proteins | Rituximab, Trastuzumab | Breast Cancer, Lymphoma |
| Cancer Vaccines | Stimulate immune response | HPV Vaccine, Provenge | Cervical Cancer, Prostate Cancer |
Immunotherapy has revolutionized cancer treatment, offering new hope to patients worldwide. By harnessing the power of the immune system, it provides targeted, durable, and innovative solutions for fighting cancer. However, continued research and personalized approaches are crucial to overcoming its challenges and expanding its benefits.
The time frame varies by patient and treatment type. Some may see results in weeks, while others may take months.
While not a guaranteed cure, immunotherapy has led to long-term remission in some cases, particularly for advanced cancers.
No, immunotherapy is most effective for certain cancers like melanoma, lung cancer, and some blood cancers. Research is ongoing for others.
Yes, patients can explore other options such as targeted therapy, chemotherapy, or clinical trials for experimental treatments.
Maintaining a healthy diet, regular exercise, and avoiding smoking can enhance overall immune function and support treatment effectiveness.
 21.12.2024
21.12.2024