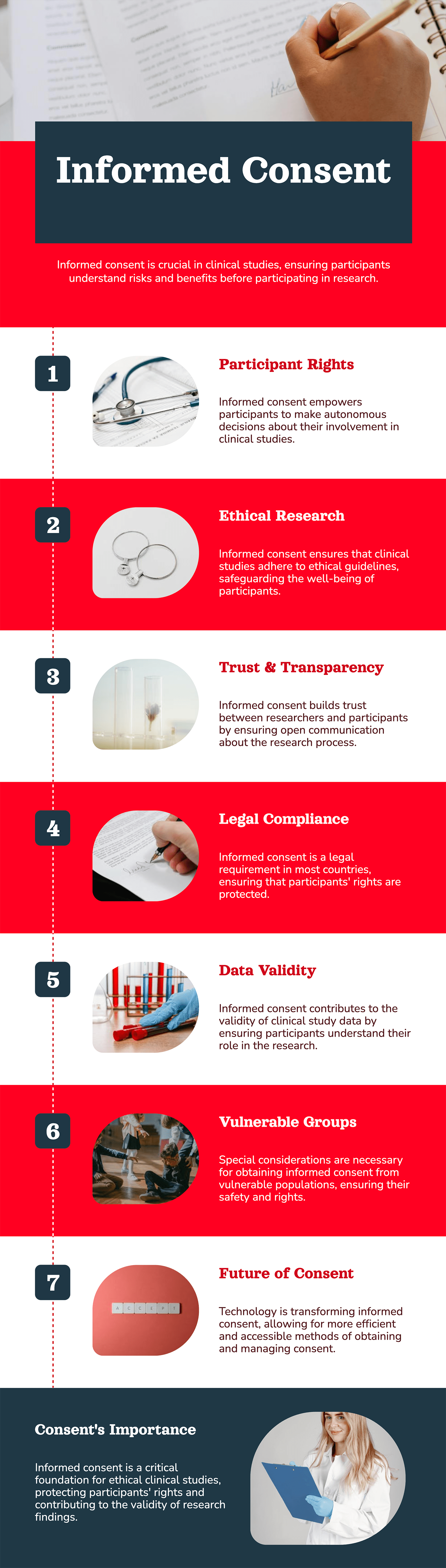
Informed consent is a cornerstone in the ethical framework of clinical study, protecting the rights of participants while being transparent between researchers and subjects. It is not just a formality; it is a process that fosters trust and encourages voluntary participation.
The importance of informed consent in clinical studies cannot be overemphasized, as it is a reflection of respect, autonomy, and ethical responsibility in medical research.
Informed consent is a process through which details of a clinical study involving its purpose, procedures, potential risks, benefits, and alternatives are given to the individuals so that they make an informed decision about being a part of it or not. The principle of informed consent in clinical studies establishes that participants are not just subjects to be experimented on but actively contribute to scientific progress through knowledge.
This procedure entails a full explanation of the study together with a form that one is expected to sign upon feeling fully and adequately informed.
This ought to be noted; consent may not necessarily be a one-time process but an open discussion between and within participants throughout the study, at which times they may withdraw at their whims.
 The core of informed consent in clinical studies is the idea of the right and freedom of an individual to control what happens to his/her body and health. One of the main ethical components of ensuring that participants join a study without being coerced, manipulated, or misinformed is autonomy. Information should be given so that the participant can freely understand what the implications of joining that study will be.
The core of informed consent in clinical studies is the idea of the right and freedom of an individual to control what happens to his/her body and health. One of the main ethical components of ensuring that participants join a study without being coerced, manipulated, or misinformed is autonomy. Information should be given so that the participant can freely understand what the implications of joining that study will be.
For instance, the participants should be given information on possible side effects, the possibility of receiving a placebo, and some financial or logistical burdens they may experience. Such empowerment of individuals is what informed consent in clinical studies protects them from exploitation and offers ethical research methods.

Informed consent in a clinical study is one aspect that is deeply rooted in the legal and regulatory frameworks of many countries all over the world. Standards such as the Declaration of Helsinki and the Belmont Report focus on the requirement to inform the participants before conducting experiments on them.
Strictly enforcing compliance with informed consent is the duty of regulatory bodies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). These standards demand that all information given to participants be clearly, accurately stated, and free from misleading statements. If not adhered to, it can bring penalties ranging from litigation and cancellation of study results.
Consent in clinical studies is therefore an important ingredient for clinical study success due to its association with trust. It enhances the participant’s perception of worth within that study when the researchers make him or her understand the objectives, risks, and possible outcomes of the study.
Transparency is also responsive to previous suspicion in biomedical research particularly among minorities. By paying attention to the principle of informed consent, clinical studies can regain confidence and increase diverse representation.
Since informed consent coupled with research material is often a tough sell, a common problem that practitioners encounter when implementing it is how to convince participants that they understand what is being said. This can be due to issues like language, illiteracy, and cultural differences all of which the patient has to overcome to understand what the doctor is saying.
To overcome these problems, the researchers can embrace creativity in their procedures; graphics, movies, and snap utilization of consent times should be embraced. As a result of the simplification of medical terms and the use of translations in participants’ local languages, it will be easier for them to understand.
Also, ensuring that the learners are allowed to ask questions or even participate in discussions gets rid of any doubts that may be in their minds and is backed by concrete data in the decision-making process.
What often happens in experiments is that ethics committees commonly referred to as the Institutional Review Boards (IRBs) help maintain the principle of informed consent in tests. These committees approve fundamental consent through the assessment of the consent process to conform with the existing and pertinent ethical standards and regulations.
The IRBs evaluate features like, whether the form used to seek consent was comprehensible, how accurate the information displayed was and the adequacy of methods used in conveying information. In this way, through analysing these elements, the privileges of ethics committees maintain participants’ rights and their safety.
Patients of a certain age, level of disability, or any other disadvantageous circumstances have to be protected in clinical studies even more. Obtaining informed consent in clinical studies for these populations entails both an assent, where possible, of the participants, and written consent from the legal mind or representative of the participant.
For instance, when conducting pediatric studies, the researchers are on most occasions required to confirm the understanding of the study by the children in their own capacity while at the same time seeking their parental consent, particularly in the case of the minors. Likewise, studies with the participation of persons with developed mental diseases will need elementary descriptions of legal actions and the presence of advocates for their defense.
As much as this document is useful when it comes to clinical studies, it is not without some challenges about the use of informed consent. One of the most frequently encountered problems is the therapeutic misconception which refers to the participants’ belief that the principal goal of the study is their medical treatment. The researchers have to pay attention to this misconception of the relevance of research and usual healthcare services.
Another issue is how to present as much data as possible, while not overloading participants with information. However, complete disclosure is mandatory while the provision of too much information may overwhelm any interested participant and cause him/her to withdraw from the process. Achieving all these is closely related to how well the authorities strike this balance and possibly organize the communication approaches.
New technologies are also changing the way of informed consent in clinical studies to become more effective and easier to carry out. E-consent systems in which the participant can review information at his/her own convenience and give consent electronically are also effective. Such platforms may use additional materials, like videos, infographics, and so on to make understanding easier.
Moreover, based on the available literature, blockchain might provide solutions to address issues of handling sensitive consent records management. As a result of using blockchain to keep records of consent, the participant’s rights are protected throughout the study.
Informed consent in clinical studies isn’t only an ethical issue when discussing whether it is right or wrong, it is a determinant of the success and quality of clinical studies.
As such, there is improved conformity to study protocol among the patients, compliance with data provisions, and honest responses. Consequently, this increases the validity of the results of the study and accelerates the approval of new therapies by the authorities.
The most promising approach to molding informed consent in future clinical research is making it even better and more dynamic in a world of emerging issues. Scholars must continue to be concerned about the ethical progressive advancements and use IT and specific approaches to improve the consent process.
The sample indicates that teamwork between researchers, Ethics committees, and patient advocacy groups will also determine the nature of the best practices. Thus, by prioritizing the multiple stakeholder involvement or, in the essence of the clinical research, the participant involvement it is possible to make a difference and protect the informed consent principle.
The concept of informed consent in clinical studies is not just an administrative process; it represents respect, integrity, and ethical behavior in research. In this way, researchers work for comprehension, autonomy, and especially transparency to gain trust and voluntary compliance.As clinical study sites continue to grow and new models developed the principle of informed consent should not be lost sight of to take advantage of the participants. This principle will remain as the beacon of ethical conducting clinical research that will enhance the growth of science with consideration of regard for the clients.
 01.12.2024
01.12.2024